The Delta variant is stronger, more formidable, and far more contagious than any strain of Covid we’ve yet encountered – and it’s forcing a rewrite of our pandemic strategy.
Communicating information during a pandemic is tricky for a number of reasons. First, it’s all based on highly technical, complex biological science that needs to be put into layman terms. Second, if it’s overly simplified, it’s unlikely to be complete. Third, if it’s not simplified enough, it’s likely to be misunderstood. Fourth, people learn, understand, and take in messaging differently. And fifth, perhaps most importantly, the science evolves along with the virus itself, so the information will by necessity change.
That last point has been a particular problem in Western countries where the Delta variant of the SARS-CoV-2 coronavirus has exploded and become the dominant strain. Most of the messaging from two or three months ago is now having to be rewritten, things like mask mandates and social distancing measures are being reintroduced, some countries are exploring the idea of making vaccination compulsory… and for people who were thinking the pandemic was largely over, none of this is going down well at all.
Plainly put, the rise of the Delta variant has forced an almost complete reset in our war on Covid-19, and has upended many things we thought we knew.
With that in mind, here are some of the more common questions, with accurate and factually based answers. Bear in mind, once again, that as the understanding of the formidable Delta variant in particular evolves, the science will reflect that, and the answers may change over time.

CAN I STILL GET COVID-19 IF I’M FULLY VACCINATED?
Yes. These are called breakthrough cases, as they ‘break through’ the protection afforded by the vaccines. It’s important, however, to understand the basics of how vaccines work. They don’t act as a shield, capably deflecting intruders, but rather as teachers, instructing and training your own body how to produce the antibodies that will fight the virus when it invades and prevent it from making you seriously ill.
Everyone’s body is a little different, and there are multiple other factors in play, too, so sometimes, despite being vaccinated, people do still get sick. If you get a flu shot (a common seasonal ritual in many cold-climate countries), you can still get the flu, but it isn’t as likely. And if you do catch it, the illness won’t be as severe, and likely won’t last as long, either.
That’s the case with the Covid-19 vaccines, but even more so. The vaccines all offer very good protection against even contracting the disease, but for the cases that do break through, almost all of those cases are asymptomatic or only mildly symptomatic.

The real-world data (which is growing every day) is overwhelming in its affirmation that the vaccines work. One of the benefits of data sets from the United States is that it’s a huge population with 50 states, each with their own rules and practices, so we can see what works and what doesn’t. It also helps (for data analysis) that there are a lot of stubborn and ignorant people who refuse to get vaccinated and therefore act unwittingly as a control group.
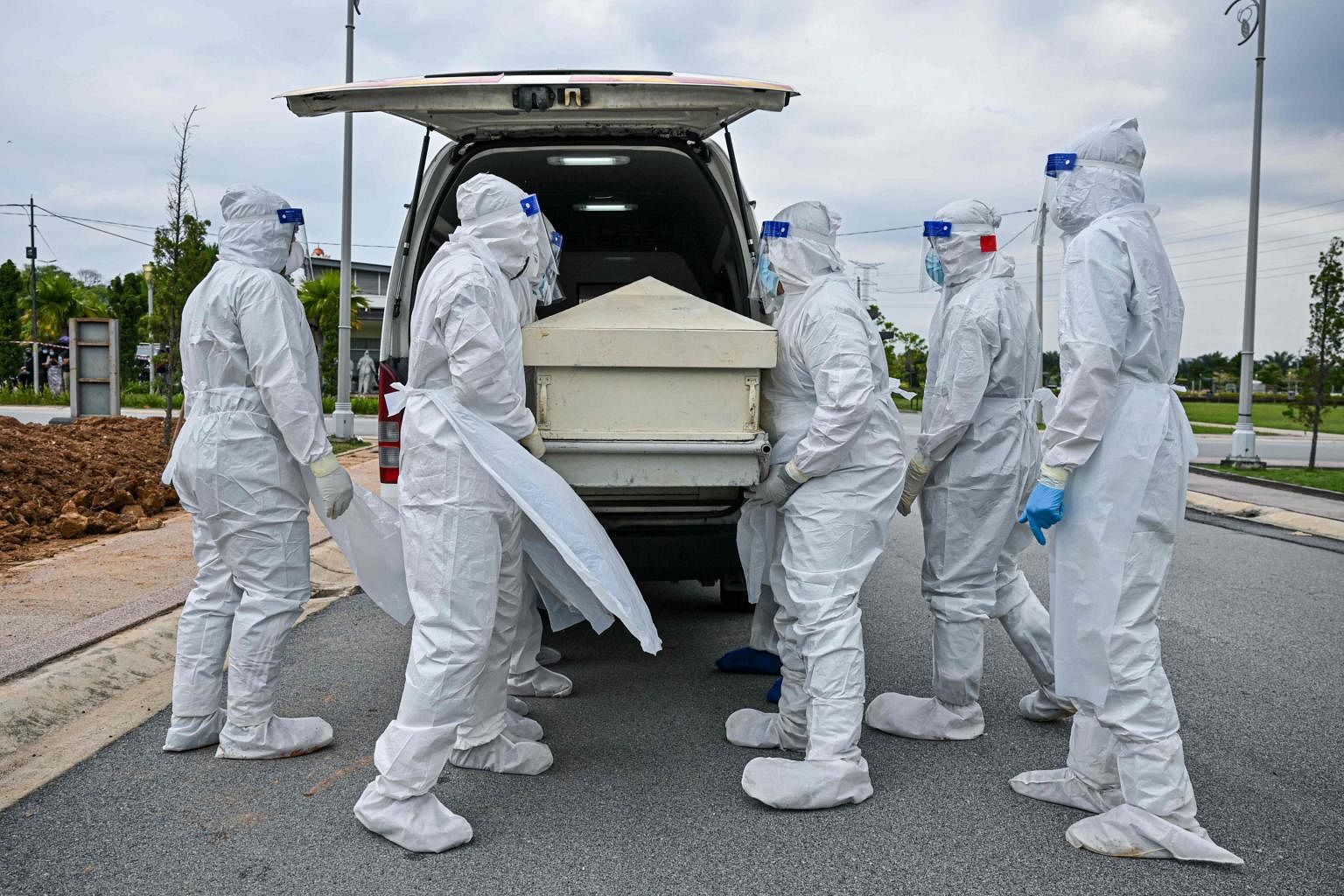
In just one example, since February in the US state of Texas (which has almost the same population as Malaysia), almost 9,000 people have died of Covid. Of those, only 43 were vaccinated, and that doesn’t even take into account their age or pre-existing comorbidities. That means the vaccines there have yielded a 99.5% survival rate against Covid. Those are pretty good odds.
More broadly, throughout the United States, the same trend is holding, with more than 99% of all Covid deaths over the past several weeks (since May) having been among the unvaccinated.
Among the vaccinated, the majority of those few who have died have been older (and male). According to researchers in the UK, the explanation for this is that the risk of death from Covid rises so sharply for the elderly and those with certain underlying health issues, that risk curve overtakes the protection curve given by the vaccine. Simply put, they say, a vaccinated 70-year-old is likely at greater risk of serious illness or death from Covid-19 than an unvaccinated 35-year-old.
We’re not aware of any peer-reviewed studies that back this assertion up, but on its face, given what we know, it seems a plausible statement.
DOES THIS MEANS THE VACCINES HAVE FAILED?
Absolutely not. No vaccine is 100% effective, but the suite of Covid vaccines we have in our arsenal honestly comes quite close. Many of them offer better than 90% effectiveness against severe illness or death. The rates of effectiveness are more variable when it comes to merely contracting the disease, but the goal here is to keep people out of the hospital, and to keep them from dying. Everything we’ve seen suggests the vaccines are doing that very effectively.

But even in the rare cases where they don’t, it doesn’t mean they’ve failed. Use the seatbelt analogy: If you buckle up every time you get in your car (as you should), you know that a seatbelt offers a certain level of protection — but it’s not 100%. So when you read an article about someone dying in a car crash, and learn that they were wearing their seatbelt at the time, do you stop wearing yours? Do you assume that seatbelts just don’t work? Of course not. People still suffer injuries and death in accidents, even though they were wearing seatbelts. But statistically, you’re far less likely to die if you’re wearing one than if you’re not. (The broad effectiveness of three-point seatbelts, which are credited with having saved well over a million lives since being introduced by Volvo in 1959, is precisely why they are mandated on every new car sold.)
The approach to vaccines is similar. Yes, there is statistically a very small risk with any vaccine, but that risk is vastly outweighed by the benefits. There is also a chance that it won’t be effective in preventing death or illness in every instance. Again, the chance is very small, and is massively overshadowed by the odds that it will be effective.
WHAT ABOUT THE VARIANTS?
Theoretically, if the world had been able to get everyone vaccinated within a few days’ time as soon as the vaccines were cleared for emergency use, we likely would have stopped the pandemic’s spread. But of course, that is utterly impossible. Since the vaccination effort has been much slower and not at all evenly distributed in the world, the virus has had plenty of time to evolve and mutate.
Every organism changes to improve its chances of survival and to pass those tiny, incremental changes down to the next generation.
Now consider a virus. Its entire purpose is to find a host, invade that host, and start replicating. Once inside its host, a virus starts making copies of itself, over and over again. In a single person, the coronavirus can replicate itself billions of times.
The longer a pandemic lingers, the more time the virus has to modify itself with each successive copy, making it more adaptable, more contagious, more fit to survive longer… so that it can make still more copies. That’s what a virus does, and it’s why variants are expected in the course of a pandemic. But though they’re expected, the form those variants take and the problems they may (or may not) pose are completely unknown. For an excellent explainer on this, click here.
So far, there appear to be four notable, identified variants to the SARS-CoV-2 virus, each named after a letter of the Greek alphabet (there is a potentially very worrisome Lambda variant in South America, but it is still being studied closely):
- B.1.1.7 (Alpha): This variant was initially detected in the United Kingdom.
- B.1.351 (Beta): This variant was initially detected in South Africa in December 2020.
- P.1 (Gamma): This variant was initially identified in travellers from Brazil, who were tested during routine screening at an airport in Japan, in early January.
- B.1.617.2 (Delta): This variant was initially identified in India in December 2020.
The fourth variant, Delta, is the one currently getting all the attention.
The biggest issue with Delta seems to be its transmissibility, but evidence is mounting that it’s also more dangerous for unvaccinated people than the original strain. As far as transmission, Delta is as contagious as chickenpox, with an R0 (“R-naught”) of about 8 to 9. That means, in an unprotected population, every infected person will infect eight or nine others, making this one of the most infectious pathogens known. The original strain of the novel coronavirus had an R0 of about 2.
Delta is altogether different. Not only is it more transmissible than any previous strain of the coronavirus, it’s also considerably more transmissible than smallpox, Ebola, SARS, or MERS, though all of those diseases have proven to be more deadly. The most contagious common disease known is measles, with an R0 of about 12 to 18. Measles has been largely eradicated in many countries due to widespread vaccination.
Remember, though, this value corresponds to spread in an unprotected community. The R0 value is less important and less useful later in a pandemic as large swathes of the population have developed immunity (through having and recovering from the disease, or from vaccines) and control measures are put in place, such as masking and social distancing.
To learn more about the known ‘variants of concern’ so far, watch the short video below (highly recommended):
SHOULD WE BE WORRIED ABOUT DELTA?
Probably so, yes. Virologists and other health experts are sounding the alarm over this fitter, faster variant, which has quickly become the dominant strain in a number of countries.
The biggest bombshell so far, however, slipped into the news last weekend, when an internal slide presentation from the US Centers for Disease Control (CDC) was released, and its authenticity subsequently confirmed: Once infected, vaccinated people can transmit the Delta variant just as easily as unvaccinated people. That’s a total game changer and likely spells an end to any fantasies of “herd immunity,” a concept which is completely predicated on curbing transmission in a population.

Also worrying is that the percentage of hospitalisations among vaccinated people is rising in some countries, though it is still BY FAR more often the unvaccinated who are contracting the disease and getting sick enough to require medical intervention. Getting fully vaccinated is still your best protection against serious illness or death. That has not changed. Infections in vaccinated people are still far less likely to occur than in unvaccinated, and the vaccines continue to be incredibly effective in preventing death or serious illness from any strain of Covid-19.
Unfortunately for us, many of the studies are coming from countries whose approved vaccines have limited overlap with those being used in Malaysia, so the data sets are usually incomplete when trying to apply them to Malaysia. (For example, the US has only one authorised vaccine in use that is also in use in Malaysia – Pfizer/BioNTech. In the UK, the Pfizer and AstraZeneca vaccines are used.)
Published studies from the US and the UK have shown compelling evidence that two doses of the Pfizer or AstraZeneca vaccine, both used in Malaysia, are highly effective against the Delta variant.
The third vaccine in widespread use in Malaysia is Sinovac, and there simply isn’t enough specific data available to determine its effectiveness against Delta. The company that produces the vaccine says it’s effective, but that’s not as valuable as an international, peer-reviewed study. What we do know from published sources is that Sinovac is highly effective against the original strain, but for now, we appear to have only the company’s word that similar levels of effectiveness extend to the Delta variant.
China is currently battling its worst surge of the virus’s spread since the pandemic began, led by a Delta-fuelled outbreak at Nanjing’s airport, which quickly spread in July.

Regardless of the specific numbers, however, the message has remained clear and consistent: Getting vaccinated is urged for all who are eligible, and is your best protection against the Delta variant.
WHAT DOES THIS MEAN?
As much as people have learned about the novel coronavirus in the past 18 months, there’s still a great deal we don’t know, and the path any pandemic will take is far from certain. For example, even now in the UK, Covid cases are plunging and though a number of theories abound, nobody really knows why. Experts are watching closely though, perhaps for any evidence that the pandemic is fizzling out in Britain, which has among the world’s highest rates of vaccination (more than 70% of adults are fully vaccinated, with 88% having had at least one shot).
The UK’s caseload now, though still high, is roughly half of what it was a little over a week ago, despite models predicting that new cases would be skyrocketing. Amid whispered talk of this being a sign the pandemic is possibly subsiding, the UK is currently whipsawing between despair and hope, not knowing what the next week with the virus will bring.
Experts seem to be fairly united on one point, however, and have been for several months: We will likely have to live with Covid-19 forever.

IS DELTA A PROBLEM IN MALAYSIA?
It almost certainly will be. Experts say it’s not a matter of ‘if,’ but ‘when.’ Delta is already here, and the number of cases is without any doubt much higher than what is officially known, a number that has been stuck at 87 for quite some time.
The strain is rampant in Asia overall, and in South and Southeast Asia particularly, so it’s unlikely that Malaysia has miraculously escaped with less than 100 cases. What is more likely is that the large surge in daily new cases is being fuelled by two things: increased testing levels and the Delta variant.
Unfortunately, Malaysia lacks sufficient genome sequencing capacity to accurately and rapidly identify specific strains of the coronavirus, but to illustrate the breathtaking transmissibility of this variant, Singapore has recorded a 99.4% increase in Delta cases in the last four weeks – nearly 900 new cases of the Delta strain. The UK has logged a similar percentage increase (99.7%) in the same period, and the Delta variant is the dominant strain there now by a significant margin, according to public health experts.
In the United States, meanwhile, Delta is exploding across the country, with the state of Florida – with its stridently anti-mask, anti-science governor Ron DeSantis repeatedly clashing with US health authorities – leading the way, setting new all-time records for single-day cases (21,683) and seven-day total hospitalisations (10,920), too. The state has fully vaccinated only about 49% of its over-12 population.
Increasingly, in countries with uneven rates of vaccination, a clear trend is emerging: Covid is becoming a pandemic of the unvaccinated. Former US Health and Human Services Assistant Secretary Brett Giroir laid it out bluntly, saying, “Anyone who is not vaccinated and who did not have Covid previously, the Delta variant is so contagious that you’re going to get it.”
In making the case for vaccines, however, Giroir added, “No matter what is being said – or what the misinformation or the confusing information is – the current vaccines are extremely effective at preventing severe disease, hospitalisations, and death, even among the Delta variant.”
Malaysia, meanwhile, has now fully vaccinated some 6.9 million people, or about 21% of its population, and it already appears to be making a difference. As you can see below, not only are more than 95% of new cases only mildly symptomatic or asymptomatic, the overwhelming majority of new cases (all categories) are being detected in unvaccinated people.

Malaysia’s vaccination efforts are still continuing at an impressive pace, so we should see millions more vaccinated by the end of August. The only question is, will it be enough, and will it be in time?
"ExpatGo welcomes and encourages comments, input, and divergent opinions. However, we kindly request that you use suitable language in your comments, and refrain from any sort of personal attack, hate speech, or disparaging rhetoric. Comments not in line with this are subject to removal from the site. "